Apologies for interrupting your experience.
This publication is currently being maintained by the Magloft team. Learn more about the technology behind this publication.
Manage your subscription to this publication here or please contact the publisher Resuscitation Council for an update.
Prevention of in-hospital cardiac arrest: the Chain of Prevention
The Chain of Prevention (Figure 2.1) can assist hospitals in structuring care processes to prevent and detect patient deterioration and cardiac arrest. There are five links in the chain:

1. Education
Education should include how to observe patients, interpretation of observed signs and signs of deterioration. It should also include the use of the ABCDE approach, simple skills to stabilise the patient until help arrives and the rationale for activating rapid response system.
2. Monitoring
Monitoring and patient assessment require the measurement and recording of vital signs, and accurate documentation.
3. Recognition
Recognition encompasses the tools available to identify patients in need of additional monitoring or intervention, including suitably designed vital signs charts and sets of predetermined ‘calling criteria’ to ‘flag’ the need to escalate monitoring or to call for more expert help.
4. Call for help
Call for help protocols for summoning a response to a deteriorating patient should be universally known and understood, unambiguous and mandated. Hospitals should ensure all staff are empowered to call for help. Call for help by using a structured communication tool such as SBARD (Situation, Background, Assessment, Recommendation, Decisions) or RSVP (Reason, Story, Vital signs, Plan).
5. Response
Response to a deteriorating patient must be assured, of specified speed and by staff with appropriate knowledge, skills and experience. Rapid response systems should be in place (e.g. from an emergency response team, critical care outreach team or medical emergency team).
Recognising the deteriorating patient
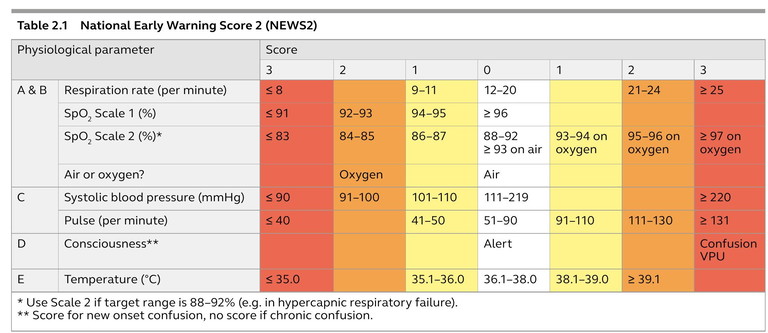
In general, the clinical signs of critical illness are similar whatever the underlying cause because they reflect failing respiratory, cardiovascular, and neurological systems (i.e. ABCDE problems, see below). To help early detection of deteriorating patients, many hospitals use early warning scores (EWS). EWS systems allocate points to measurements of routine vital signs based on their deviation from an agreed ‘normal’ range. The weighted score of one or more vital sign observations, or the total EWS, indicates the level of intervention required (e.g. increased frequency of vital signs monitoring, or the need to call ward doctors or resuscitation teams to the patient). In the UK, the National Early Warning Score 2 (NEWS2) is recommended (Table 2.1).
Figure 2.1 The Chain of Prevention
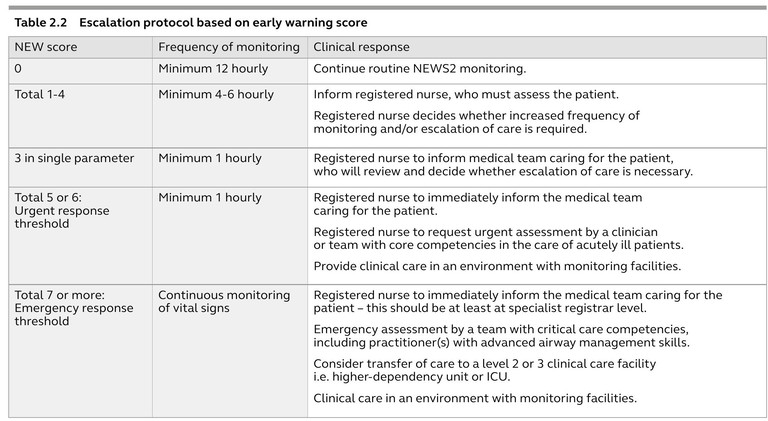
EWS are dynamic and change over time and the frequency of observations should be increased to track improvement or deterioration in a patient’s condition. If it is clear a patient is deteriorating, call for help early rather than wait for the patient to reach a specific score.
The patient’s total EWS is calculated as the sum of physiological parameters as seen in Table 2.1. An increased score indicates an increased risk of deterioration and death. There should be a graded response to scores according to local hospital protocols. An example of escalation plan is shown in Table 2.2.
Alternatively, systems incorporating calling criteria are based on routine observations, which activate a response when one or more variables reach an extremely abnormal value. Research suggests that EWS may be better discriminators of outcomes than calling criteria. Some hospitals combine elements of both systems.
Nurse concern may also be an important predictor of patient deterioration. Even when doctors are alerted to a patient’s abnormal physiology, there is often delay in attending to the patient or referring to higher levels of care.
Resuscitation Council
We're with you for life.
Resuscitation Council UK is saving lives by developing guidelines, influencing policy, delivering courses and supporting cutting-edge research. Through education, training and research, we’re working towards the day when everyone in the country has the skills they need to save a life.
Categories
Explore our inspiring content by topic